Disease in the Civil War
by Dr. Bonnie Brice Dorwart
A variety of diseases afflicting Civil War soldiers caused significantly more casualties than battle.
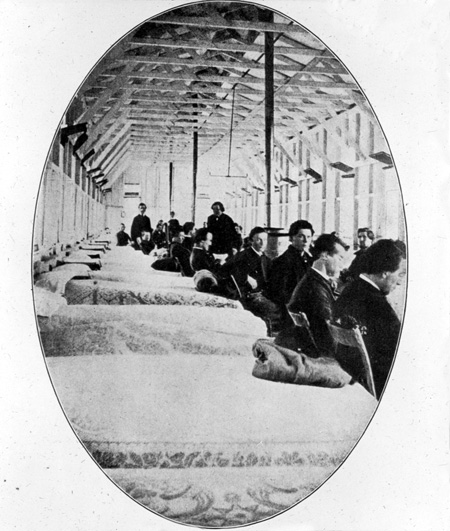
Most readers of the American Civil War have the impression that soldiers of the time suffered chiefly from wounds, and amputations without anesthesia. Partly this reflects literature written for the public during the past fifty years in the pre-digital era when primary sources never contained an index and commonly had a scanty—if any—table of contents. Furthermore, pictures of amputations, wounds, and prosthetic devices are far more dramatic and capable of being photographed (cameras of the time required static images with long exposure times). There were no video cameras to record the much less interesting and mundane scenes of men passing diarrheal stools, vomiting, sweating with fever and delirium, coughing exhaustively with bronchitis, or bedridden with rheumatism or abscesses. Moreover, the role of surgery in the war, authored by surgeons, dominated medical writing available to the public.[1]
With digitization of primary sources, especially the massive 50 pound Medical and Surgical History of the War of the Rebellion in 1990-91, the “Sickness and Mortality Reports” recorded by the Union Army could finally and practically be analyzed. This record of 150 diagnoses of non-hospitalized patients contains only 14 related to wounds, and includes troop numbers at risk as well as outcome (death or recovery) for each illness of each month and year of the war. This material details the illnesses, their causes and treatment, and the rationale for such care. Its conclusion, illustrating medical knowledge of the time, allows the reader to see diseases through the eyes of the surgeons (all physicians were called surgeons during the war) who ministered to their men.[2]
Whether one reads surgeons’ personal journals from the period, official reports of the surgeons general or even generals of both armies, the refrain is the same: sickness is everywhere. This, from the U.S. Sanitary Commission, is typical, poetic, and sad: “Disease, insidious and inevitable, is now stealing through the camps…menacing our dearest treasure—the nation’s youth.”[3]
Of the 700,000 soldiers who died, more than 400,000 perished with sickness.
Why and what types of illness might we predict? There are four characteristics of every army that influence public health in wartime: enlisted men are males 20 to 30 years old; they live in crowded circumstances; environmental conditions in the field are primitive; military objectives sometimes override sanitary ones.[4]
The armies who fought in the U.S. Civil War were comprised largely of Caucasian males who grew up in relative isolation on farms. Not having experienced the common diseases of childhood, the new soldiers fell prey to them as adults. General Robert E. Lee wrote his wife in August 1861, “The soldiers everywhere are sick. The measles are prevalent throughout the whole army….” By September 1, battle readiness is still hobbled by infected troops. Those on the sick-list would form an army”, Lee went on. He underscored how severe measles in the adult can be: Measles, “though light in childhood is severe in manhood, and prepares the system for other attacks.” Lee was correct about measles in the adult. In a 1991 report to the Center for Disease Control and Prevention (CDC), complications were more common in patients older than 20 years than in children. Of 3,220 military recruits with measles between 1976 and 1979; 3% developed pneumonia, requiring hospitalization, 17% had bronchitis, 31% hepatitis, 29% middle ear infection, and 25% sinusitis.[5]
Regarding field conditions and over-riding military concerns, unsanitary conditions were common during the war. There are frequent references to the interplay of flies, fingers, feces, and food.
Joseph Jones, M.D., the Confederate surgeon inspecting the Andersonville stockade in Sumter County, GA, wrote of one stream filled with “the filth and excrement of twenty thousand men, the stench was disgusting and overpowering; and if it was surpassed in unpleasantness by anything, it was only in the disgusting appearance of the filthy, almost stagnant, waters moving slowly between the stumps and roots and fallen trunks of trees and thick branches of reeds, with innumerable long-tailed, large white maggots, swollen peas, and fermenting excrement, and fragments of bread and meat.”[6]
Joseph Janvier Woodward, M.D., Surgeon U.S. Army, documented the same breaches of sanitation in camps. “In great armies in time of war personal cleanliness is often… [nonexistent.] The men [are] unwashed, their clothes filthy, bodies full of vermin, and heaps of garbage [lie] about….” “Especially [needed] was…policing the latrines. [The] trench is…too shallow [not the requisite five feet deep], daily covering…with dirt is entirely neglected.” “Large numbers of the men will not use the sinks [latrines] …but instead every clump of bushes [and] every fence border.” It is impossible to step outside the encampment without having “both eye and nostril continually offended.”[7]
John Strong Newberry, M.D., of the U.S. Sanitary Commission (U.S.S.C.) in late 1861 reported contamination of even the water supply. The latrine “is the ground in the vicinity, which slopes down to the stream, from which all water in the camp is obtained.”[8]
Clearly there is evidence that lack of sanitation was widespread and responsible for much of the illness among troops in both armies. Interestingly, it was not because the relationship between sanitation and disease was unknown at the time of the Civil War that lapses of sanitation occurred. The sanitary reform movement preceded the war, evolving between 1800 and 1860, with publication of such works as the Shattuck report of 1850. [9]
One reason for poor sanitation was a lack of discipline in many camps, perhaps because surgeons were not aware of implications for health, or were so busy with twice daily Surgeons’ Call where troops in camp reported for sick bay. Maybe surgeons were too overwhelmed, no matter how much help was sought or received, to ensure the daily burial of dead horses and their dung. Attention to the shocking prevalence of poor sanitation is one reason the United States Sanitary Commission—a non-governmental agency—was formed and approved by President Lincoln early in the war. A telling reference to camp conditions in Cairo, Illinois, in the same USSC report reads, “The horses and mules are invariably kept too near the camps, and the daily removal of their dung is a myth dreamed of only by the authors of the army regulations and the Sanitary Commission Inspectors.” It was not uncommon for an army of 50,000 men to be accompanied by 15,000 horses and mules, with the latter excreting 30 pounds of feces each day. Undoubtedly, a final factor was the recognition by several observers that neat, clean camps had the same number of ill soldiers with the same illnesses as dirty, unkempt ones. Obviously, if hand-washing by troops and surgeons had been recognized as a singularly critical activity in preventing and controlling disease, the results might well have been different.[10]
To summarize: if the common contagious diseases of childhood did not strike down soldiers, diseases spread by flies, fingers, feces, and food did. These, of course, are illnesses caused by bacteria that maximize reproduction when humans and unsanitary conditions coexist. Diarrhea, dysentery, typhoid fever, and food poisoning with bacteria such as Salmonella are direct consequences of unsanitary practices. For those spared childhood infections or those associated with poor hygiene, malaria could be counted on to cause dangerous fevers and liver disease whenever stagnant water abounded.
The cause of malaria and its transmission by the anopheles mosquito was not determined until 1897, three decades after the Civil War ended. Numerous accounts attest to the presence of the vector, although it was recognized only as a nuisance at that time. From the USSC Report #69 of 1863, it is clear that mosquitoes were such an aggravation to the troops immediately after the Battle of Gettysburg that the great expenditure of $810 for 649 pieces of mosquito netting was warranted.
What did the generals of the U.S. Army and the C.S. Army think the role of medical officers was? Union surgeon, Jonathan Letterman, Medical Director of the Army of the Potomac for 18 months, believed it was to provide his commanders with healthy soldiers who can win the war: “A corps of Medical officers was not established solely for the purpose of attending the wounded and sick…. The leading idea…is to strengthen…the commanding General by keeping his army in the most vigorous health, thus rendering it…efficient for enduring fatigue, privation, and fighting [emphasis added].” Confederate surgeon, J. Julian Chisholm, author of A Manual of Military Surgery (1861) wrote, the “fire of an enemy never decimates an opposing army. Disease is the fell destroyer of armies, and stalks at all times through encampments. Where balls have destroyed hundreds, insidious diseases, with their long train of symptoms, and quiet, noiseless progress, sweep away thousands. To keep an army in health is, then, even more important than to cure wounds from the battlefields.”[11]
The diseases that incapacitated soldiers and hampered their commanding officers most commonly from the inception of the war through the first year after its end are shown in Tables 1 and 2.
Let’s look at the five most common illnesses in detail.
Diarrhea/Dysentery
The natural history of diarrhea/dysentery, especially during war, has been understood only since 1945. Diarrhea is frequent watery stools that can cause shock and death without replacement of fluid and chemicals required for the body to function. Dysentery is the same entity, but with bloody stools. Conditions that favor them and their infectious agents are similar. Ingestion of food or water contaminated by feces containing certain strains of Shigella or Salmonella bacteria, but not the Salmonella that causes typhoid fever, results in diarrhea or dysentery. Patients recovering from these usually pass bacteria in their stools for 7 to 10 days. The greatest danger in this type of dysentery is from carriers with chronic dysentery, or from mild and unrecognized disease.[14]
This type of dysentery is spread to healthy individuals from carriers who harbor and excrete the bacteria in their stools, but do not themselves have diarrhea or dysentery. Flies living outdoors play a crucial role in spreading diarrhea/dysentery. They appear about ten days after climate becomes favorable for their breeding; they disappear with the onset of severe frost. Since 1912 house flies were proven to carry bacillary (rod-shaped bacteria listed above) dysentery, contaminating food by vomiting or defecating on it after feeding on dysenteric stools. Hairs on fly legs in contact with infected material are the most common conveyers of the bacteria to food, probably because they provide a much larger surface area to which the bacteria can cling. Water from contaminated wells is another source. Since 1918, it has been known that Shigella survive and increase in stored water, and that chlorination is incapable of rendering contaminated water safe, but the dysentery organisms are destroyed quickly by direct exposure to sunlight.[15]
A more meaningful indicator of the seriousness of diarrhea and dysentery is provided by the number of cases occurring in every thousand men, as shown in Table 3. How effectively could an army march or fight, especially as numbers of soldiers increased after the first (full) year of the war, if 850 of every 1,000 were bed-ridden or severely weakened with diarrhea or dysentery?
Fevers
Causes of the fevers that affected more than one million white troops and 150,000 USCT were mainly typhoid fever, malaria, and rheumatic fever―all debilitating, long-lasting, and potentially fatal conditions.
Typhoid fever typically causes the body temperature to rise steadily and continuously over weeks or even months, exceeding 104°F. Also common are severe weakness, lack of appetite, headache, mental confusion, red flushing of the face, nosebleed, bronchitis, abdominal pain with constipation or diarrhea (but not dysentery), enlarged spleen, and sometimes a rash on the abdomen and chest (rose spots). Caused by the bacterium, Salmonella typhi, it occurs only in humans. Without antibiotics, death may occur. Survivors shed living Salmonella typhi in their stools that can be passed to others via hands unwashed after a bowel movement, even if there are no symptoms of infection as occurred in the famous case of Typhoid Mary. These stools can contaminate water also.[18]
Of the 79,462 cases of typhoid fever listed in The Medical and Surgical History of the Civil War (MSHCW), only 119 detailed reports appear there. Of these, 44 men received mercury as part of their treatment. Details of Private George Barber’s typhoid fever appear below. He survived and returned to duty 27 days after his disease began. Barber was one of 51 soldiers from the Army of the Potomac treated for typhoid fever in the Seminary Hospital, Georgetown, D. C., in late 1861. Death rate of this series was 19.6 percent.[19]
Case 9. —Deafness; dizziness, but mental faculties clear; diarrhea; rose colored spots on the 10th and 12th days, fading on 14th, when convalescence followed; to duty on 27th day. —Private George N. Barber, Co. G, 14th N. Y.; age 18; was admitted Sept. 20, 1861, …sick a week before with weakness, pains in the head, back and bowels, and epistaxis [nosebleed]. Diagnosis—typhoid fever. On admission the pulse was 114, the skin hot and moist, the face flushed, …with irritability of the stomach and much tenderness in the right iliac region [right lower part of the abdomen]; the patient was sometimes affected with dizziness, but his mind was clear. Blue-pill [mercury, liquorice root, confection of roses] was given. On the 21st he had five stools…, anorexia [loss of appetite], a slight cough…. On the 22d the epistaxis recurred…; pulse 76. Quinine in eight-grain doses was given three times daily, with morphia [an opiate] at night. … [T]here was a steady improvement, and the patient was returned to duty October 9.[20]
Malaria also causes a high fever, but it is intermittent, not constant. If fever in malaria occurs every three days, it is called quartan; if every two days, tertian; if daily, quotidian. Because the parasite (plasmodium) that causes malaria ruptures the red blood cells in which it grows and reproduces, the patient becomes anemic and pale. Liver involvement may cause yellowing of the patient’s skin (jaundiced; icteric). Surgeon Joseph J. Woodward gives an insightful description of the disease in his 1864 book; “The complexion is…icteroid in hue, and a peculiar anemic pallor, with the evidences of hepatic disorder, permits at once the recognition of…chronic malarial poisoning.” Civil War surgeons connected the disease to hot weather and standing water and believed its cause to be vapors (mal air) arising from rotting vegetation. Not until 1897 was its correct cause and transmission worked out by Sir Ronald Ross: a parasite living in a specific mosquito (Anopheles) is inserted via a mosquito bite into a human from another human already infected with malaria. Although the MSHCW records 982,611 cases of malaria (defined as Intermittent Fever: Quotidian, Tertian or Quartan), there are detailed records of only 102 soldiers with malaria. Of these, 21 were prescribed mercury by their surgeons in the U.S. Army. One case illustrates course of disease and treatment.[21]
Case 4. A quartan with slow recovery after several relapses, Private James Wright, Co. F, 21st Ill. Vols.; age 21; was admitted September 25, 1863, having a chill every third day. His skin was sallow, tongue coated and bowels loose. Strychnia, blue-pill [mercury rubbed with confection of roses, beaten with powdered liquorice root] and capsicum [derived from peppers] were prescribed. He improved slowly…with several relapses; ultimately Fowler’s solution [arsenic and potassium; used as an alterative, intended to alter the natural history of a disease without obvious loss of a bodily substance] proved effectual and the patient was returned to duty February 14, 1864. —General Hospital, Quincy, Ill.[22]
There is no evidence that arsenic kills the causative parasite. The surgeon assumed that because the soldier improved after arsenic, this treatment was the reason why. Before controlled studies were used to test medical treatments, such assumptions commonly established medical practices. Quinine, an effective treatment, was used widely during the Civil War to treat malaria. This case is unusual in that Private Wright was not given quinine.
Rheumatic fever will be discussed in the next section, on rheumatism.
Rheumatism
Rheumatism was the third leading reason that troops could not march or fight, responsible for 254,738 cases, with 475 deaths among white troops and 32,125 cases causing 235 deaths in USCT. Again, we gain better appreciation of the impact by looking at cases per 1000 troop strength.[23]
Having 10 to more than 25 per cent of one’s army affected poses a serious handicap, especially when many types of rheumatism have prolonged and crippling courses. Because there are 44 case reports, detailed clinical descriptions of “rheumatism,” and autopsies on such patients in the Medical and Surgical History of the War of the Rebellion, it is possible to hypothesize what rheumatic diseases plagued the troops. Considerable guesswork is involved in doing so, because surgeons’ descriptions are often few and sketchy, and because a given patient may be suffering from more than one disease or entity at the same time. Nonetheless, the following are likely candidates.
“Rheumatism” is a very old term, connoting pain, stiffness, and limited motion of joints, because of disease arising in joints themselves or in muscles, tendons, ligaments or bones attached to them. “Arthritis” is a very specific term that denotes swelling, pain, warmth, and variable redness in a joint, with resulting loss of the ability to fully bend, straighten or rotate the joint. “Rheumatic disease” applies to structures other than merely the joints, e.g., tendons, bursas, muscles. Presently more than 100 distinct types of rheumatic disease are recognized.
Rheumatic fever has doubtless been a scourge to the military for a very long time, since it is spread by close contact in crowded quarters. Not until World War II was its transmission limited by the simple step of arranging soldiers’ cots in head-toe alternation in their quarters. At the same time the cause of rheumatic fever was recognized as an abnormal immune response in a patient whose throat was infected by a bacterium, a Group A streptococcus, resulting in a particular type of “strep throat.” An equally important discovery―made by growing strep in the laboratory from recruits with a sore throat and those without one―was that a critical number of positive strep cultures resulted in rheumatic fever. Without penicillin, which did not come into use until 1943, neither treatment nor prophylaxis of rheumatic fever would have been possible.
This disease develops in 3% of untreated cases of Group A strep throat infections two to four weeks later. It involves the heart, has a characteristic arthritis and skin rash, nodules in the skin, and jerking movements of the limbs (chorea) weeks to months later, first described by Cheadle in 1889. Criteria that allow us to define this disease more accurately were developed by T. Duckett Jones in 1944, and modified in 1992. A probable case follows, written in the terse style of reporting surgeons of the time.[25]
Case 1. P.H., no age given. Admitted 1–24–1862, with back pain and sore swollen ankles; left knee involved too, but not described, duration unknown. Pulse elevated, hot skin. Pain disturbed sleep. 24 hours later ankles still very painful, although only slightly swollen, “but right knee hot, swollen and painful; pulse accelerated; skin hot.” At 48 hours “both knees hot and…swollen, but the right only painful; ankles sound…; pulse 80.” Three days after admission “pain only in the left knee, which is enlarged from effusion [fluid in the joint]; pulse about 60, very irregular; skin hot; pain in the region of the heart. Five days after admission rested well; appears well; pulse regular….” Discharged 6th day to quarters. Treated with colchicum. Duration of rheumatic symptoms: 6 days (?). Hospital 28th Mass.[26]
Although thermometers were known at the time of the Civil War, body temperature of patients is almost never recorded. As in this case, skin of patients with fever is usually simply described as “hot.” The migratory pattern of the arthritis in rheumatic fever is typical, as swelling subsided in his ankles, and moved to his knees. An irregular pulse is common, and may lead to death; in soldier P.H. it became regular at time of his discharge. “Pain in the region of the heart” was probably pericarditis, an irritation of the lining around the heart, often with accumulation of fluid, which if voluminous enough, may kill the patient. Colchicum, derived from the autumn crocus, is used today to treat several types of rheumatic disease, but not rheumatic fever. Note that he was not returned to duty, but to his quarters. With involvement of his heart, he probably would have required a period of light activity in camp before resuming active duty.
Arthritis following dysentery/ diarrhea or after non-gonorrheal urethritis
(reactive arthritis) was experienced by some unfortunate soldiers who endured diarrhea or dysentery, the intestinal infection was followed by an immune reaction one week to one month later—leading to sudden painful swelling in several joints, to genital and skin rashes, and to conjunctivitis, possibly with involvement of the iris of the eyes resulting in blindness. The same abnormal immune response to the rod-shaped bacteria causing dysentery/ diarrhea occurred in some patients after sexual relations with a partner infected with a different microorganism, possibly one called Chlamydia. In these cases a purulent (pus-like) discharge from the urethra is seen, similar to that of sexually acquired gonorrhea. Since the mechanism by which post-dysentery/diarrhea and post-non-gonorrheal urethritis produce arthritis, conjunctivitis/iritis, and rashes is a reaction to a previous infection, this type of arthritis is referred to as reactive arthritis. A case report follows:
Case 40. A.T.H., age not given. 8–7–1864: “Diarrhoea for a few days. Gave anodynes and astringents [like black oak bark causing tissues to contract and tighten].” 8–14 “Diarrhoea persisting; articular rheumatism manifested in the lumbar region and in right knee.” 8–21 “Easier; some debility.” 8–31 Inflamed eye “recurring;…flakes…in aqueous humor [fluid in the eyeball]; iris hazy and sluggish; cornea clouded; vessels much injected.” 9–16–1864 discharged from service for severe visual impairment. Kansas City Hospital, Mo.[27]
Most of the more than 100 types of arthritis known to affect humans are not inherited. However, many who develop arthritis after Shigella and Salmonella-induced diarrhea or dysentery are born with a gene called Human Leukocyte Antigen-B27 (HLA-B27). Arthritis after such intestinal infections occurs more often in those with the gene. Furthermore, they may develop diarrhea, urethritis, arthritis and conjunctivitis (sometimes) repeatedly for up to 10 years after the inciting infection. Since persons of African descent almost never carry the HLA-B27 gene, and most of the soldiers during the Civil War were Caucasian, reactive arthritis probably comprised much of the rheumatic disease that occurred in both armies. As if the patient suffering reactive arthritis did not have enough to deal with, he also had an increased chance of developing another serious type of arthritis, ankylosing spondylitis.
Deforming Arthritis of the spine (ankylosing spondylitis, AS) typically begins in adolescent males, and almost always before age 35, with gradual pain and stiffness in the lower back. It is also associated with the HLA-B27 gene. Unlike mechanical back pain relieved by bed rest, that of AS requires the patient to walk around to relieve the pain. He also is beset with anemia, fatigue, weight loss and, potentially, blindness. Untreated, the arthritis may deform the hips, shoulders and knees. A hallmark of the disease is permanent fixation of the back bones in a forward bent-over position from the neck to the tailbone―the “poker spine.” Obviously, there was no effective therapy.
There are descriptions of this disease in Civil War troops, such as this superb one by Joseph Woodward: Disease begins “with malaise, languor, and …indisposition to exertion.” “Vague pains…appear in various portions of the body,”…but their most common seat is in the thighs and legs, and in the small of the back.” “As the disease progresses…pain becomes more severe, and…the patient becomes quite unfit for duty.” “A peculiar pallid, clay-like appearance of the countenance, a tendency toward emaciation, palpitation of the heart—especially after any exertion…are among the most constant symptoms.”[28]
The arthritis of scurvy (scorbutic arthritis) is discussed below.
Tuberculosis was well known to doctors of the time, especially with its propensity to deform and destroy the spine, causing Pott’s Disease. One percent of patients infected with tuberculosis will develop infection of the spine or other joints. Tuberculosis, like rheumatic fever and other chronic rheumatic conditions, made it impossible for a prospective soldier to serve in the military. Union surgeon John Ordronaux explained how to examine for Pott’s disease; “This affection is one of very serious consequence, in a military point of view. It reveals itself by a prominence and bulging of the spinous process [bony knob along the back of the spine], corresponding to the vertebra which is its seat…. [T]o discover the disease, the patient must be made to bend forward, while the hand is passed over the spine, to test its sensibility, and to examine critically any abnormal protuberances or depressions which may be encountered.”[29]
Since the causative bacterium of tuberculosis was not discovered until 1882, diagnostic skin tests until 1890, x-rays for diagnosis until 1895, and effective treatments (streptomycin, para-amino salicyclic acid, isoniazid and ethambutol) in 1944, 1946, 1952 and 1961, respectively, not only soldiers of the Civil War often were maimed or died from their infection, but also those of subsequent wars.
Septic arthritis (pus in a joint), with or without a wound, was common, many bacteria having been introduced via simple skin abrasions, or through wounds inflicted by missiles. One case shows that drainage of the pus was the only option surgeons had:
Case 44. C.M.D. age 22. Admission date not given, but incision over right hip area was done in June, 1862, evacuating “about two quarts of pus….” Onset occurred after “several hours in the rain” on 4–18–1862, with “severe pain in his right hip, the whole of the gluteal region becoming swollen, tense and tender; some fever …[accompanying] the local inflammation.” By 9–1862 “abscess had healed” but pain made patient “unable to bear his weight on the limb….” He also had dullness over lower half of right chest, and rales with dullness in left lung and a [cardiac] murmur. Discharged 9–1862. Duration of rheumatic symptoms: longer than 5 months. Hospital, Quincy, Ill.[30]
The consequences to this soldier would have been dire. He would not be able to walk without assistance. Likely he had pneumonia in his left lung, and his heart murmur suggests that bacteria, having escaped into the bloodstream, would have been destroying a heart valve.
Gonorrheal arthritis occurs with two patterns. Gonorrhea is a sexually transmitted disease (STD), caused by a bacterium called gonococcus, usually between heterosexuals. Males develop severely painful penile swelling and discharge soon after contact, with painful swelling of a single joint, commonly a knee, a few days later. Invariably this soldier seeks help at Surgeon’s Call in his camp. Until penicillin became available, treatment was limited to instillation of various liquid (useless) solutions into the urethra and/or catheterization to allow passage of urine through a urethra obstructed by the infection. The joint was often destroyed. A second pattern was recognized and described in the late 20th Century, occurring in men having sex with men. Because gonococci are deposited in the pharynx or the anus, very few symptoms may occur, allowing the infection to spread into the bloodstream. This results in swelling and pain often in both wrists (often with tendonitis), and blood blisters on the fingers and toes. Both patterns can be deadly without antibiotics.
Surgeon John Ordronaux was aware of sexually transmitted arthritis, writing the following in 1863, “Arthritis…, when simple and recent, justifies neither rejection nor discharge [from military service] whatever may have been…its origin, whether accidental or gonorrheal [emphasis added], with the exception…of…the shoulder or hip joint, which are often serious, and demand all the attention of the surgeon. These diseases, when chronic, are…always causes for rejection, and sometimes…discharge.”[31]
Syphilis, another STD, can also cause arthritis. Caused by a microscopic germ known as a spirochete, this infection is extremely complex. A few weeks after sexual exposure, a primary stage occurs. The hallmark of this period is a genital ulcer called a chancre. It is associated with swollen lymph glands in the groin. The chancre is highly infectious to the owner (and any sexual partner). If primary syphilis is not treated with systemic antibiotics secondary syphilis results. Physicians of the Civil War period were aware of, and characterized well, the first stage of this infectious disease. Bumstead describes primary syphilis: “There is always an interval between the appearance of the chancre and of the general manifestations of syphilis. This period of incubation of general symptoms…is fixed within certain bounds, like the incubation of other infectious diseases. Its average duration is six weeks….”[32]
What they did not, nor could not, know was that the spirochete spreads very quickly to the bloodstream, and spreads internally beyond the chancre within hours or days of infection, even before the chancre appears. It is during this stage of secondary syphilis that arthritis may appear, along with mouth and skin rashes, fever and swollen lymph glands throughout the body. Dr. Bumstead gives an equally insightful picture of secondary syphilis: “Early general symptoms…consist of an eruption of blotches…upon the skin, …mucous patches…of the mouth…general malaise [sense of not feeling well], headache, and fleeting pains in various parts of the body, [more particularly in the neighborhood of the joints].”[33]
Secondary syphilis has been associated with joint pain and swelling in several reported series. Ankles and small joints of the feet were the most common in a report in 1916. Swelling and pain in one joint, or both knees predominated in another, published in 1932. Further manifestations, latent and tertiary syphilis, unknown to Bumstead et al are beyond the scope of this section.[34]
Rheumatoid arthritis is usually a devastating long-lasting and deforming form of arthritis, effective treatment of which became available only in the late 20th Century. Care of this condition during the War is illustrated by this case report:
Case 5. A.M. age 52. Admitted 4–5–1864, “suffering from rheumatism while at home on furlough. Knees and wrists swollen and painful....” By 4–9 needed a narcotic. 4–26 swelling and pain “much diminished.” June 1 arms and hands very swollen, until June 15 when “somewhat reduced.” By July 28 regaining “use of arms slowly; wrist-joints stiff.” Diagnosis “acute rheumatism.” Feb. 18, 1865, discharged “because of chronic rheumatism causing distortion and deformity of joints of fingers of both hands and left knee-joint.” Treated with Dover’s powder [opium and ipecac], colchicum, potassium iodide, iron, quinine, joints packed in lint soaked in sodium bicarbonate, wet cupping “drawing about an ounce and a half of blood,” pressure bandages warm bath, external
tincture of iodine. South Street Hospital, Philadelphia, Pa.[35]
Opium was given by mouth, dusted onto skin over painful joints or injected via syringe and needle. Ipecac, was used to induce sweating in cases with inflammation (swelling, warmth, redness, pain) or fever, believed to remove injurious substances from the blood. Cupping supposedly removed them by drawing blood into a blister formed by suction of the glass “cup.” Quinine was given not only for malaria, but also for other causes of fever. Aconite (wolfsbane, or monkshood) was employed as a sedative if given by mouth; as an irritant if applied to the skin. Colchicum (colchicine) remains a useful treatment today for several rheumatic diseases.
Malarial rheumatism was described in 1976 as having fever, muscular aching, backache and joint pain. Although there are no case reports of this entity during the War, it clearly was recognized. Surgeon A.H. Lanphier, 106th Illinois Infantry, wrote from Jackson, TN in 1862, “Resident physicians tell me they have more rheumatism and intermittent fever than all other diseases together. I suppose that the low swampy surface of the country will account for this fact. It is customary here to give large doses of quinine in acute rheumatism, and the practice is by no means unsuccessful.” Civil War surgeons connected malaria with hot weather, marshes, and standing water, believing it to be caused by vapors (mal air) arising from decaying vegetation. As discussed above not until 1897 was the cause of malaria finally established.[36]
The arthritis of gout is exceedingly painful, caused by the explosion of tiny very sharp needles of uric acid in one or more joints. Ordronaux, as always, is on target. In 1863, he says, “Gout is extremely rare in youth, being generally found only in old age.” “It is also …infrequent… among soldiers and non-commissioned officers, whatever may be their age. It would, if present, constitute a disqualification for the military service.” There were fewer than 500 cases in all white troops in the entire Union Army and fewer than 10 in the USCT.[37]
Miscellaneous causes include mumps. Arthritis occurs with this viral infection in less than 1% of cases and more frequently in men. “The arthritis begins from day 1 to 15 days after the onset of the… [swelling and pain in the parotid glands] with multiple large and small joints affected.” Large collections of fluid in the joints are uncommon. Symptoms subside within two weeks, “although arthritis may persist for up to 3 months.” There were 48,128 cases of mumps in white troops and 12,186 in USCT.[38]
There are some references to rheumatic diseases in the Confederacy, as well. “A major in the Jeff Davis Legion seeks reassignment to an Alabama regiment so that he will not have to winter in Virginia. Over a year of campaigning and sleeping on wet ground has caused him great suffering from rheumatism.” “The number of men [in hospital] has risen again…during November, largely because the winter weather has produced new cases of pneumonia, rheumatism, and like ailments….”[39]
Abscesses
Abscesses were the fourth most common reason why white union soldiers could not march or fight. Treatment was incision and drainage, using thread as a drain. Sometimes a “seton wound” was made by passing thread or wire through the skin into an abscess, creating a passage to drain the pus. The seton sometimes was left in place for the rest of the soldier’s life, depending on the location of the abscess. Of course, drainage was not done with sterile technique or materials, because the role of microscopic living particles in causing infection was unknown to the surgeons. It is remarkable therefore that of more than a hundred thousand abscesses, there were only 180 deaths reported in the Sickness and Mortality Reports for the entire war in white soldiers and of 6,000 in U.S.C.T., only 21 deaths.[40]
Scurvy
The arthritis of scurvy (scorbutic arthritis) occurs when foods containing vitamin C are not eaten and was the fifth most common reason soldiers could not march and fight. It causes bruising of the skin, but more importantly, painful bleeding into joints and under the periosteum (lining around bones), especially the knees, ankles and shins. Obviously a soldier so affected would not have been able to stand up, much less march. Surgeon General of the Union Army (April 1862 to August 1863) William Hammond described his findings in soldiers and its treatment:
“Scurvy was known to the ancients, cured, as at present, by the use of fresh vegetable food. [Those with scurvy have] swollen and discolored gums, bleeding patches of…blood, first upon the legs…; hardness and [a] permanent state of contraction of the muscles; …stiffness of the joints; …reopening of old ulcers and cicatrices [scars].… Stiff joints [should be] rubbed with a stimulating liniment and be forcibly extended and fixed by mechanical means (splints to straighten them).”[41]
Unfortunately much of the food of both armies was dehydrated or overcooked, destroying any naturally occurring vitamin C. Especially tragic was the finding of a study in 1940 that showed the Minimum Daily Requirement of vitamin C to be a measly 30 mg/day.
Conspicuous by their absence in the present writing, are details of the same diseases in the Confederate States Army (CSA). Sadly, when Richmond was burned at the end of the War, its medical records were lost almost in their entirety.
If you can read only one book:
Dorwart, Bonnie Brice. Death is in the Breeze: Disease during the American Civil War (Frederick, Maryland: National Museum of Civil War Medicine Press, 2009).
Books:
Adams, George W. Doctors in Blue: The Medical History of the Union Army in the Civil War, (New York: Henry Schuman, 1952).
Bayne-Jones, Stanhope. The Evolution of Preventive Medicine in the U.S. Army, 1607–1939 (Washington, D.C.: Government Printing Office, 1968).
Bollet, Alfred Jay., Civil War Medicine: Challenges and Triumphs (Tucson, AZ: Galen Press, 2002), chap.6.
Chisholm, J.J. A Manual of Military Surgery, for the Use of Surgeons in the Confederate States Army (Columbia, SC: Evans and Cogswell, 1864).
Cunningham, H. H. Doctors in Gray: The Confederate Medical Service, (Baton Rouge: Louisiana State University Press, 1958).
Dunglison, R. A Dictionary of Medical Science (Philadelphia: Lea and Blanchard, 1846).
Gillett, Mary C. The Army Medical Department, 1818-1865 (Washington D.C.: Government Printing Office, 1987), chaps.7-13.
Letterman, J. Medical Recollections of the Army of the Potomac. (New York: Appleton, 1866).
Steiner, Paul E. Disease in the Civil War: Natural Biological Warfare in 1861-1865 (Springfield, IL: Charles C. Thomas, 1968).
Straubing, Harold E. In Hospital and Camp: The Civil War Through the Eyes of Its Doctors and Nurses (Mechanicsburg, PA: Stackpole, 1993).
Woodward, J.J. Outlines of the Chief Camp Diseases (Philadelphia: J.B. Lippincott, 1863).
Organizations:
National Museum of Civil War Medicine
The NMCWM is the only non-governmental museum devoted to Civil War Medicine in the United States. The museum contains exhibits, vintage tents and ambulances. It holds an annual meeting with peer-reviewed abstracts and it operates the NMCWM Press. 48 East Patrick Street Frederick, MD 21705 (301) 695 1864. 10:00-5:00 M-S, 11:00-5:00 Sun.
Society of Civil War Surgeons
The specific goal of The Society of Civil War Surgeons is to promote, in both members as well as the general public, a deep and abiding appreciation for rich medical heritage of the American Civil War. Peer reviewed papers are published quarterly and an annual meeting is held with peer reviewed abstracts.
Web Resources:
No web resources listed.
Other Sources:
No other sources listed.